
How does UChicago Medicine help patients with a blood clot? Through UChicago Medicine’s comprehensive PE and DVT program, we routinely treat patients with high risk blood clots using advanced technologies to dissolve or remove the blood clot, using minimally invasive methods with short recovery times. However, a small percentage of patients will need additional treatment. Most blood clots can be managed simply with blood thinners. Your medical provider will likely do imaging exams such as an ultrasound of the leg or, for concerns of a PE, a CT scan of the lungs. It is important to be evaluated immediately if you experience symptoms of a blood clot. What should you do if you think you have a blood clot? This can be very debilitating, and it’s sometimes not recognized by non-vascular specialists.
Blot clot in leg skin#
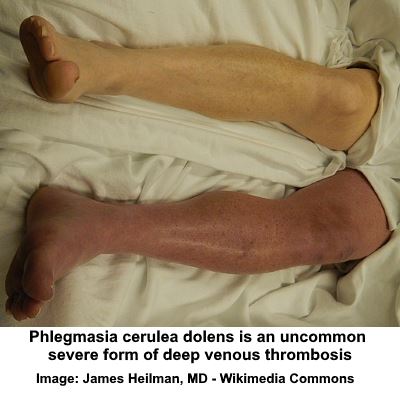
That doesn’t mean the blood doesn’t get back to the heart, but the blockage can cause leg swelling, pain and skin changes, such as darkening or ulcers. If that occurs, then there is essentially a blockage of the blood flow back to the heart. If a DVT is left untreated, there may be scarring of the veins in the legs and abdomen. What happens if a blood clot goes untreated? In some cases, blood clots may cause permanent damage to blood vessels. Our bodies have their own innate mechanisms to dissolve blood clots.

If you believe you may have either a DVT or PE, it is important to see a doctor immediately. A PE typically causes shortness of breath, chest pain, dizziness or extreme fatigue. DVT can be silent, but some people experience limb pain, swelling or discoloration of the skin. Only a medical provider can make the diagnosis, using imaging tests performed in a hospital or office. How do you know if you have a blood clot? A PE can be life-threatening and can cause symptoms such as shortness of breath, chest pain, rapid heart rate, dizziness or excess fatigue. When a blood clot forms in the large veins in the legs (a DVT), it can break off and travel through the bloodstream to the lungs, a condition known as pulmonary embolism (PE). In certain cases, however, the clot does not resolve and continues to grow in size. Most of the time, the body can dissolve a clot on its own. If you get hurt, a blood clot usually forms to stop the bleeding. Blood clots may form in response to a number of conditions, such as an acute illness, immobility or inflammation. This information applies to everyone, but is especially important for people infected with COVID-19.Ī blood clot forms when liquid blood coagulates and becomes a semisolid, gel-like structure inside a blood vessel. Here are a few basic facts about blood clots, the symptoms, and what you should do if you think you might have one.

“It’s likely a direct effect of COVID-19,” said Paul, UChicago Medicine’s PERT director and an interventional cardiologist. Early in the pandemic, hospitals in New York City reported a 30% rate of blood clots among ICU patients with COVID-19, a percentage well above normal for patients who are critically ill. UChicago Medicine is actively studying strategies to prevent and manage COVID-19-related blood clotting. In some patients, this can include damage to the lungs, heart, kidneys and/or brain. Studies are underway to learn more about COVID-19’s lasting impacts on the body. While not all of them had COVID-19, the doctors attribute part of the uptick in volume to the virus. Similarly, the volume of patients with large blood clots in the legs (also known as deep vein thrombosis, or DVT) has increased significantly, said vascular and interventional radiologist Osman Ahmed, MD. UChicago Medicine’s Jonathan Paul, MD, said the Pulmonary Embolism Response Team, or PERT, saw a 75% increase in cases last year (from 154 in 2019 to 270 in 2020). Doctors at the University of Chicago Medicine have seen a sharp increase in large blood clots found in the legs and lungs of people with COVID-19, including younger patients who typically don’t experience them.


 0 kommentar(er)
0 kommentar(er)
